Audiometry is a key hearing test in audiology. It checks how well you can hear different sounds. This test is vital for spotting hearing loss, which affects about 30 million adults in the U.S.
It uses terms like sound frequency and hearing loss diagnosis. These terms are important in understanding how we hear.
Sound intensity is measured in decibels (dB). It goes from a whisper at 20 dB to a jet engine’s roar at 140-180 dB. Sound tone, or the speed of sound waves, ranges from low bass at 50-60 Hz to high-pitched sounds at 10,000 Hz or more.
Our normal hearing range is 20-20,000 Hz. Most of our speech falls between 500-3,000 Hz.
Audiometry is key in finding hearing loss. It affects 25 percent of people between 51 and 65 years old. Over 50 percent of those over 80 years old also have hearing loss. Young people, especially those who listen to loud music, are also at risk.
Key Takeaways
- Audiometry is a non-invasive hearing test that measures sound intensity and tone.
- Nearly 30 million American adults have some degree of hearing loss.
- Sound intensity is measured in decibels (dB), ranging from a whisper at 20 dB to a jet engine at 140-180 dB.
- Sound tone is measured in Hertz (Hz), with normal human hearing ranging from 20-20,000 Hz.
- Audiometry is crucial for diagnosing hearing loss in patients of all ages.
Introduction to Audiometry
Audiometry is key in hearing tests. It checks how well we hear and can spot hearing problems early. Audiologists use special tools to find out how much hearing loss there is. They then suggest treatments like hearing aids.
Definition of Audiometry
Audiometry measures how well we hear sounds. It tests if we can hear different sounds clearly. The goal is to find the softest sound we can hear, measured in decibels.
There are many types of audiometry tests. Pure tone audiometry and speech audiometry are common. Each test looks at different parts of our hearing.
Importance of Audiometry in Hearing Assessment
Audiometry is crucial for catching hearing loss early. It helps find the right treatment, like hearing aids. This improves our quality of life and how we communicate.
It also finds out why we might have hearing problems. This could be from loud noises, age, or certain diseases. Knowing this helps choose the best treatment.
| Sound Level (dB) | Example |
|---|---|
| 20 | Whisper |
| 80-120 | Loud music (some concerts) |
| 140-180 | Jet engine |
Audiometry is important for everyone, at any age. It’s especially vital for older adults. Regular checks help keep our hearing sharp as we age.
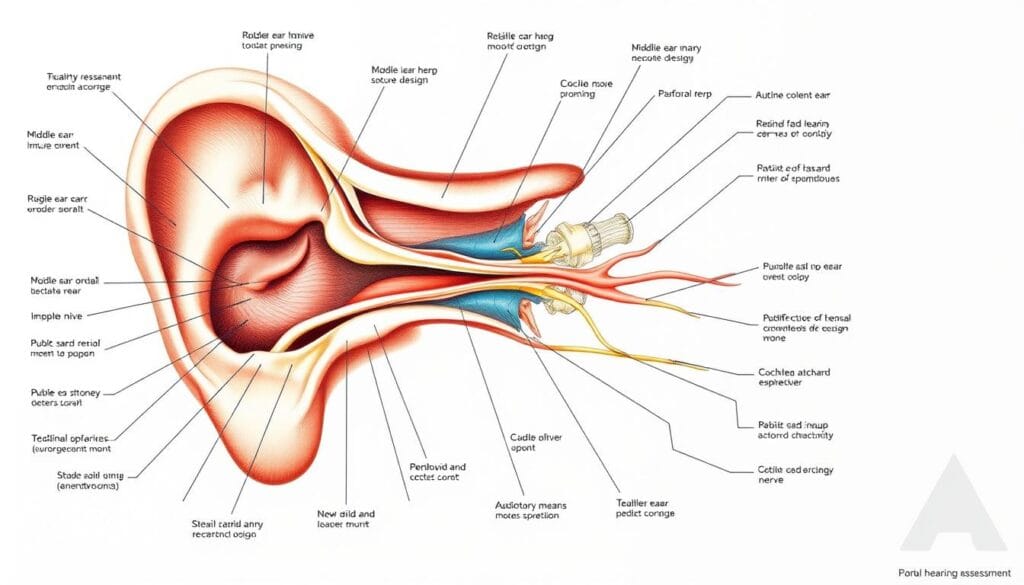
Anatomy and Physiology of the Ear
The ear is a complex sensory organ that helps us hear and balance. Knowing how the ear works is key for accurate audiological evaluations and diagnosing hearing issues. It has three main parts: the outer ear, middle ear, and inner ear. Each part has a unique role in hearing.
Outer Ear
The outer ear includes the pinna (the visible part) and the external auditory canal. The pinna collects and directs sound waves into the ear canal. This canal leads to the eardrum.
The outer ear is also where people often get piercings. However, cartilage piercings can heal poorly. African-Americans are 15 times more likely to get keloids from ear piercings than whites.
Middle Ear
The middle ear is filled with air and has three tiny bones: the malleus, incus, and stapes. These bones transmit vibrations from the eardrum to the inner ear. The eustachian tube connects the middle ear to the throat, balancing pressure.
Otitis externa, an inflammation of the external auditory canal, can affect the middle ear if not treated.
Inner Ear
The inner ear includes the cochlea and the vestibular system. The cochlea has hair cells that convert sound vibrations into electrical signals. These signals go to the brain via the auditory nerve.
The human ear is most sensitive to sounds between 1,000 and 4,000 hertz. We can hear sounds from about 20 to 20,000 hertz.
| Frequency Range | Location in Cochlea |
|---|---|
| 20 Hz | Apex of the cochlea |
| 20 KHz | Base of the cochlea, close to the round and oval windows |
The vestibular system, including the semicircular canals and otolith organs, helps us balance and stay oriented. Trauma, like what boxers experience, can cause cauliflower ear. This is a deformity of the pinna from scar tissue.
The unit of Hertz measures the frequency of sound waves in terms of cycles produced per second. Most auditory stimuli contain a mixture of sounds at various frequencies and intensities.
Understanding the ear’s anatomy and physiology helps healthcare professionals diagnose hearing disorders. This knowledge is key for effective treatment and managing hearing loss.
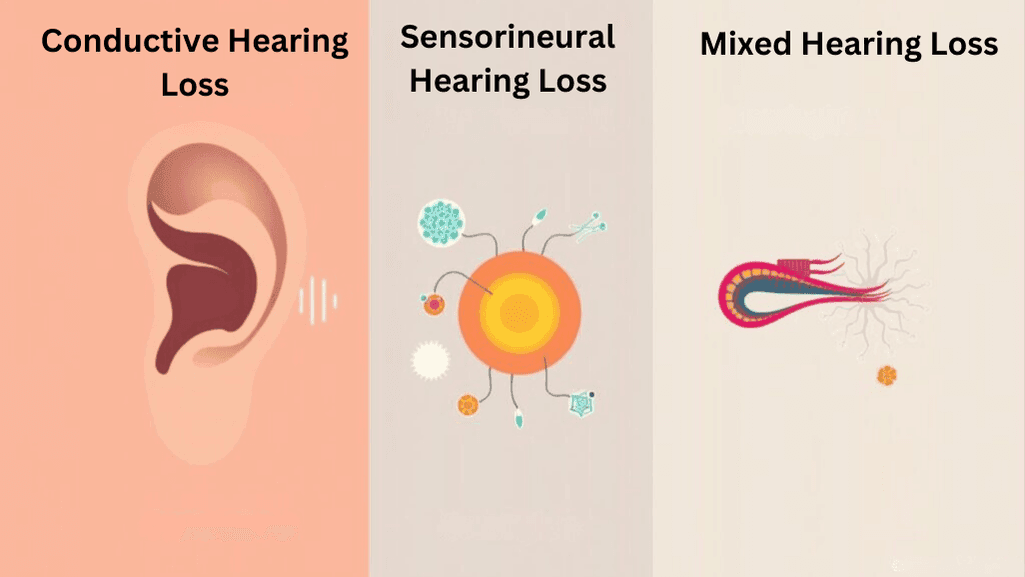
Types of Hearing Loss
It’s important to know the different types of hearing loss. Audiologists divide it into three main types: conductive, sensorineural, and mixed. Each type needs special hearing tests and treatment plans.
Conductive Hearing Loss
Conductive hearing loss happens when the outer or middle ear has a problem. This stops sound from reaching the inner ear. Causes include:
- Earwax buildup
- Ear infections
- Perforated eardrum
- Ossicular chain discontinuity or fixation
This type of hearing loss is common in kids. It can be due to ear infections or putting things in their ears. Tests like tympanometry help find the problem.
Sensorineural Hearing Loss
Sensorineural hearing loss (SNHL) affects the inner ear or the auditory nerve. It’s the most common type. It can be caused by:
- Aging (presbycusis)
- Noise exposure
- Ototoxic medications
- Genetic factors
- Head trauma
Age-related hearing loss, or presbycusis, gets worse with age. It’s very common after the age of 70. Some medicines can also cause permanent hearing loss.
Tests like pure tone audiometry help find out how bad SNHL is.
Mixed Hearing Loss
Mixed hearing loss has both conductive and sensorineural parts. It happens when there’s a problem in the outer or middle ear and damage to the inner ear or nerve. Causes include:
- Chronic ear infections
- Otosclerosis
- Head trauma
- Genetic factors
Tests like pure tone audiometry are needed to find out the cause of mixed hearing loss.
| Type of Hearing Loss | Prevalence |
|---|---|
| Sensorineural Hearing Loss | Most common type of hearing loss |
| Conductive Hearing Loss | Most common in children |
| Presbycusis (Age-related Hearing Loss) | Prevalence doubles every decade from 2nd to 7th decade of life |
| Noise-induced Hearing Loss | Accounts for 16% of adults worldwide with disabling hearing loss |
Audiometry Medical Terminology
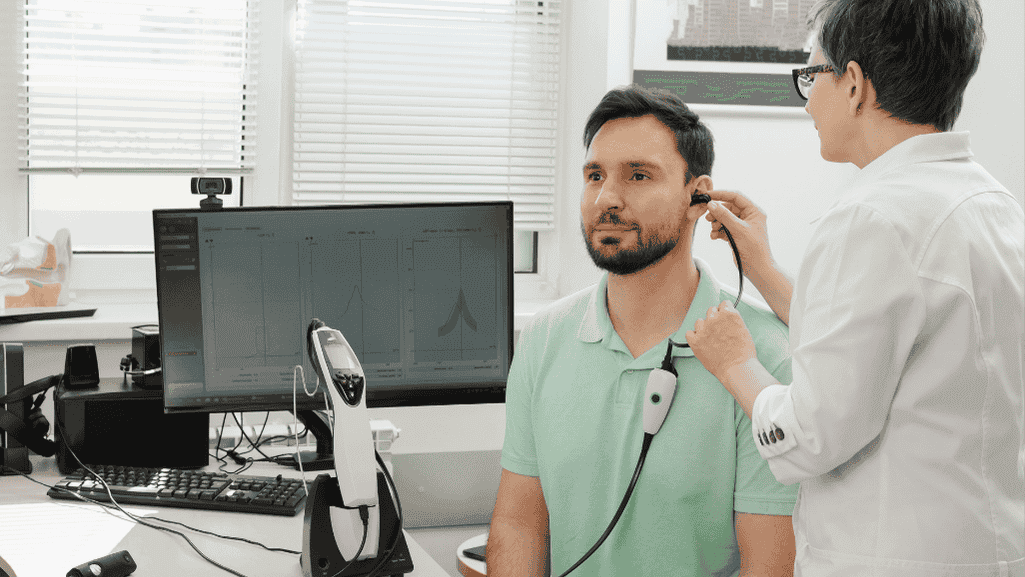
Audiometry is key in audiology. It involves tests to check hearing and find hearing loss or disorders. Knowing the terms used in audiometry is important for health care workers and those who want to keep their hearing good.
Pure Tone Audiometry
Pure tone audiometry is a common test. It checks how well you can hear different sounds. Humans can hear sounds from 20 to 20,000 Hertz and from 20 decibels up.
During the test, you wear headphones and tell when you hear a sound.
Speech Audiometry
Speech audiometry tests how well you understand speech at different volumes. It finds your speech reception threshold and speech discrimination score. These are key for diagnosing hearing loss and picking the right hearing aids.
This test is great for seeing how hearing loss affects daily talk.
Tympanometry
Tympanometry checks the middle ear’s function and pressure. It gives info on the eardrum and ossicles. The test uses air pressure in the ear canal and measures the eardrum’s response.
It’s important for finding middle ear problems like fluid buildup or eustachian tube issues.
Acoustic Reflex Testing
Acoustic reflex testing checks the stapedius muscle’s contraction to loud sounds. This reflex protects the inner ear from loud noises. Abnormal reflexes might show nerve or brainstem problems, or hearing loss.
Otoacoustic Emissions (OAE)
Otoacoustic emissions (OAE) testing looks at the outer hair cells in the cochlea. These cells are key for hearing. OAEs are sounds made by the cochlea and can be measured with a probe in the ear canal.
Missing or weak OAEs might mean hearing loss or damage to these cells.
Auditory Brainstem Response (ABR)
Auditory brainstem response (ABR) testing checks how signals travel from the cochlea to the brainstem. It’s a non-invasive test good for infants, young kids, and those who can’t do regular audiometry. ABR can spot problems like neuropathy, tumors, and disorders in the auditory pathway.
An audiometry exam can take from five to ten minutes for a quick check or up to an hour for a detailed one. Audiologists with advanced degrees can accurately diagnose and manage hearing issues like conductive loss in kids, noise-induced loss, presbycusis, and sensorineural loss in adults.
Pure Tone Audiometry
Pure tone audiometry is a key ear test to check hearing at different sound levels. It uses pure tones at specific decibel levels to find hearing thresholds for air and bone conduction. This helps audiologists understand the type and degree of hearing loss, which is vital for monitoring ototoxicity and planning treatments.
In a pure tone audiometry test, the patient sits in a sound-treated booth with earphones. The audiologist plays pure tones at various frequencies, from 250 to 8000 Hz, and increases the decibel level until the patient hears the sound. This is done for both air and bone conduction, using earphones and a bone oscillator on the mastoid bone.
The test results are shown on an audiogram, a graph that displays hearing thresholds. The audiogram helps the audiologist see the patient’s hearing sensitivity. It shows the degree and type of hearing loss based on air and bone conduction thresholds.
| Degree of Hearing Loss | Decibel Range (dB HL) | Impact on Hearing |
|---|---|---|
| Normal Hearing | 0–25 dB | Hearing is within normal limits |
| Mild Hearing Loss | 26–40 dB | Causes inattention and difficulty suppressing background noise |
| Moderate Hearing Loss | 41–55 dB | Affects language development and interaction with peers |
| Moderate-Severe Hearing Loss | 56–70 dB | Leads to difficulty with speech and decreased speech intelligibility |
| Severe Hearing Loss | 71–90 dB | Affects voice quality |
| Profound Hearing Loss | >90 dB | Results in speech and language deterioration |
Pure tone audiometry helps diagnose the type of hearing loss. It can be conductive, sensorineural, or mixed. Conductive loss shows poorer air conduction than bone conduction. Sensorineural loss has similar air and bone conduction thresholds. Mixed loss combines both.
Accurate pure tone audiometry is key for early detection and treatment of hearing loss. It’s especially important for children and those at risk for ototoxicity. Regular tests help identify changes in hearing and guide treatment options like hearing aids or cochlear implants. This ensures the best hearing health and quality of life.
Speech Audiometry
Speech audiometry is key in hearing tests. It shows how well someone can hear and understand speech. Audiologists use it to find the lowest sound level a person can hear words at, called the speech reception threshold (SRT). They also check how well a person can understand words using special lists.
This helps audiologists understand a patient’s hearing better. They can then make treatment plans that fit the patient’s needs.
Speech Reception Threshold (SRT)
The SRT is a crucial part of speech audiometry. It’s the lowest sound level a person can repeat 50% of words correctly. In tests, the SRT should be close to the average of pure tones at 500, 1000, and 2000 Hz.
This makes sure the hearing test results are reliable. People with normal hearing usually have an SRT 10-15 dB better than their pure tone average. This shows a strong link between these two important measures.
Speech Discrimination Score
Speech discrimination testing is vital in speech audiometry. It checks how well a person can repeat words at sound levels above their hearing threshold. Tests use word lists like PB-50 and NU-6.
These tests are done at levels that are easy to hear, with and without hearing aids. The score shows how well a person can understand speech. This helps in planning treatments and fitting hearing aids.
| Speech Audiometry Test | Description |
|---|---|
| SPIN (Speech Perception in Noise) | Consists of 8 lists of 50 sentences with varying predictability levels presented at different signal-to-noise ratios |
| QuickSIN (Quick Speech-in-Noise) | Effective in verifying open-fit behind-the-ear hearing aids |
| HINT (Hearing in Noise Test) | Measures speech recognition thresholds in both quiet and noise through reception thresholds for sentences |
| WIN (Words-in-Noise) | Determines the signal-to-babble ratio for normal and impaired hearing using monosyllabic words in multitalker babble |
| BKB-SIN (Bamford-Kowal-Bench Speech-in-Noise) | Utilizes Americanized BKB sentences and is designed for children and cochlear implant candidates/recipients |
Speech audiometry has grown since the 1920s and 1930s. Big steps were made after World War II because of hearing loss in veterans. Now, most audiologists use speech tests for everyone.
They use standard materials and make sure patients know the test words. This makes the tests more accurate. It helps in making better diagnoses and treatments for hearing problems.
Tympanometry and Acoustic Reflex Testing
Tympanometry and acoustic reflex testing are key parts of a detailed auditory assessment. They give important insights into how well the middle ear works and the health of the hearing pathway. These tests work together with other methods like pure-tone audiometry to help doctors understand and treat hearing problems.
Tympanogram Types
Tympanometry checks the middle ear’s mobility and air pressure. It does this by changing the ear canal’s pressure and measuring sound changes. The results show different middle ear conditions through various types of tympanograms:
- Type A: Normal middle ear function
- Type B: Flat tympanogram, suggesting fluid in the middle ear or a perforation in the tympanic membrane
- Type C: Negative peak pressure, indicating Eustachian tube dysfunction or middle ear pathology
- Type As: Shallow peak, suggesting a stiff middle ear system or otosclerosis
- Type Ad: Deep peak, indicating a flaccid or hypermobile middle ear system
Tympanometry is very good at predicting middle ear problems, with a 49% to 99% predictive value. It’s especially useful when combined with symptoms, showing a 90% sensitivity and 75% specificity in diagnosing otitis media with effusion (OME).
Acoustic Reflex Thresholds
Acoustic reflex testing checks how the stapedius muscle reacts to loud sounds. It shows how well the hearing pathway works from the middle ear to the brain. Normal hearing people usually have reflex thresholds between 70-100 decibels (dB) sound pressure level (SPL).
But, abnormal reflex thresholds can mean different problems:
| Condition | Acoustic Reflex Findings |
|---|---|
| Conductive Hearing Loss | Higher acoustic reflex thresholds, correlating with the degree of hearing loss |
| Sensorineural Hearing Loss | Normal or slightly elevated thresholds, especially in mild-to-moderate cases with recruitment |
| Facial Nerve Disorder | Elevated or absent reflexes (>100 dB SPL) |
| Middle Ear Disorder | Elevated or absent reflexes (>100 dB SPL) |
| Type B Tympanogram | Reflexes may be absent or not recordable |
Using both pneumatic otoscopy and tympanometry enhances the accuracy of diagnosing middle ear effusion, with professional tympanometry and pneumatic otoscopy demonstrating the highest sensitivity at 93.8% for diagnosing OME.
By adding tympanometry and acoustic reflex testing to the diagnosis, doctors can better find and treat middle ear problems. They can also tell the difference between conductive and sensorineural hearing losses. This helps in creating specific treatment plans for hearing disorders.
Otoacoustic Emissions (OAE) and Auditory Brainstem Response (ABR)
OAE and ABR are key parts of hearing tests. OAEs are sounds made by the cochlea’s outer hair cells. They help us understand the inner ear’s function. Some people might hear these sounds as tinnitus.
For newborns, tests like transient-evoked and stimulus-frequency OAEs are used. These tests help check if a baby can hear.
DPOAEs are great for finding high-frequency hearing loss. They work best between 2000 Hz and 8000 Hz. A specific setup helps tell if someone can hear normally or not.
OAEs are good at spotting mild hearing problems. They show if the cochlear amplifier and outer hair cells are working right.
OAE is used in the universal newborn hearing screening program (UNHS) widely adopted in North America, Europe, and developed countries, in combination with ABR testing.
ABR tests how sound travels from the ear to the brain. It uses electrodes on the head to record responses. A normal ABR has five waves at set times.
In the U.S., ABR waveforms are plotted with the vertex site as positive. This shows I, III, and V peaks.
| ABR Wave | Clinical Significance |
|---|---|
| Wave I | Associated with hearing outcomes in idiopathic sudden sensorineural hearing loss (ISSNHL); smaller amplitudes at suprathreshold levels in individuals with normal pure-tone auditory thresholds but a history of greater noise exposure |
| Wave V | Most often analyzed in clinical applications; believed to originate from the vicinity of the inferior colliculus; systematic decrease in latency in preschoolers aged 3.12-4.99 years, indicating continued development through preschool years |
| Wave VI | Lower activity in the right-side ABR wave VI in children with attention deficit hyperactivity disorder (ADHD) prior to methylphenidate treatment compared to when treatment had reached a steady state |
OAE and ABR together give a full picture of hearing. DPOAE monitoring shows changes in the cochlea. OAE also helps with diagnosing problems in the brain’s hearing system.
Interpreting Audiometric Results
Understanding audiometric results is key in the audiologic evaluation process. It gives insights into how well someone can hear and if they have hearing loss. The main tool used is the audiogram, a graph showing hearing levels during the test.
The audiogram shows hearing levels for air and bone conduction at different frequencies. These frequencies range from 250 Hz to 8000 Hz. Sounds are measured in decibels (dB), from the softest at 0 dB to the loudest at 120 dB.
Audiogram
The audiogram uses circles or triangles for the right ear and Xs or squares for the left. This makes it easy to compare hearing between the two ears. Normal conversation is about 60 dB, and hearing levels below 25 dB for adults and 15 dB for babies are considered normal.
The audiogram also includes speech tests. These tests show how well someone can understand and recognize speech at different volumes.
Identifying Type and Degree of Hearing Loss
Audiologists use the audiogram to find out the type and degree of hearing loss. There are three main types: conductive, sensorineural, and mixed. Conductive loss shows higher air conduction thresholds and an air-bone gap. Sensorineural loss has elevated thresholds for both air and bone conduction with little or no gap. Mixed loss is a mix of both.
The degree of hearing loss is based on how severe the threshold elevations are. Here’s a table showing the different degrees and their threshold ranges:
| Degree of Hearing Loss | Threshold Range (dBHL) |
|---|---|
| Normal Hearing | -10 to 14 |
| Slight Hearing Loss | 15 to 25 |
| Mild Hearing Loss | 26 to 40 |
| Moderate Hearing Loss | 41 to 55 |
| Moderately-Severe Hearing Loss | 56 to 70 |
| Severe Hearing Loss | 71 to 90 |
| Profound Hearing Loss | 91+ |
Hearing loss can come from many things, like loud noises, certain medicines, head injuries, or disorders. For example, being exposed to 85 dB sounds for a long time can cause hearing loss. This is often shown as a “notch” at 4000 Hz on the audiogram.
Audiologists use audiometric results to diagnose hearing loss and suggest treatments. This includes innovative sound therapies or devices to help with hearing. It’s important to understand the audiogram well to give the best care for those with hearing problems.
Conclusion
Audiometry is key in otology for checking hearing and finding hearing loss types. It helps doctors understand how well patients can hear. This lets them give the right treatment.
Modern audiometer tools have come a long way since the 19th century. Today, they can measure hearing very accurately. This helps doctors to see how well a person can hear.
Getting your hearing checked often is important. It helps find hearing problems early. Tests like pure tone audiometry and speech audiometry give doctors important information.
These tests show how well a person can hear. They help doctors know what kind of hearing loss there is. This guides how to treat it.
As technology in audiometry gets better, doctors need to keep learning. They must know the latest in otology and how to use new tools. This way, they can give the best care to people with hearing problems.